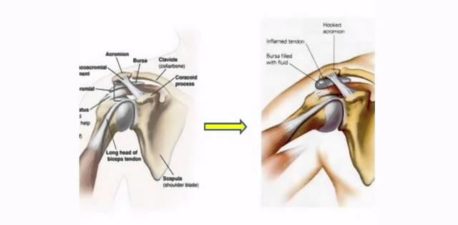
Patients suffering from severe shoulder pain know that it can impact every aspect of life, from mobility to sleep to the ability to perform basic daily tasks like getting dressed or pushing a grocery cart. The shoulder is a ball and socket joint, comparable to the hip, and has a greater range of motion than any other joint. It’s made up of three bones: the humerus (upper arm), scapula (shoulder blade), and clavicle (collarbone), which converge at the socket. The head of the humerus is the “ball” that fits into the glenoid cavity, the “socket” part of the scapula, and is stabilized by a ring of cartilage called the glenoid labrum. Damage to this protective cartilage can cause the bones to rub together, leading to joint pain that can be debilitating.
Damage to the shoulder joint can occur as a result of osteoarthritis, rheumatoid arthritis, rotator cuff tear arthropathy, or bone deterioration caused by restricted blood (avascular necrosis), among other conditions. For patients who haven’t found relief with non-surgical treatments like physical therapy or steroid injections, shoulder replacement surgery may be recommended. The outpatient procedure involves making an incision to access the shoulder joint. The surgeon then removes the damaged cartilage or parts of bone, and replaces them with metal and/or plastic implants.
X-rays have traditionally been used to assess a patient’s shoulder before replacement surgery, but x-ray doesn’t provide a comprehensive view of the joint. Now, some orthopedic surgeons–including our own Dr. Noerdlinger–have embraced a state-of-the-art technology called Exactech Guided Personalized Surgery that creates a detailed 3D model of the shoulder joint. The visual map allows the surgeon to plan and virtually simulate the surgery in advance, and utilize computer-assisted guidance during the procedure. The replacement surgery can be tailored according to the individual patient’s unique anatomy, allowing for optimal implant placement. Exactech GPS enhances precision and accuracy, resulting in better functionality, fewer complications, and an expedited recovery process.
Specializing in shoulder surgery (both Arthroscopic & Shoulder Replacements), our own Dr. Noerdlinger has been voted Top Orthopedic Surgeon by New Hampshire Magazine every year from 2017 to 2023. Dr. Noerdlinger performed 140 replacement surgeries in 2023 and is recognized as one of the top shoulder surgeons in New England. Below, he answers some questions about Exactech GPS.
In your own words, how does this procedure benefit your patients?
The Exactech GPS system allows surgeons to place the shoulder replacement in the most accurate position, which improves outcomes.
Who is a good candidate for Exactech Guided Personalized Surgery?
Anyone considering a shoulder replacement.
Where do you perform this procedure?
I perform the surgery at NECOS and at York Hospital.
Anything else you’d like current or future patients to know about this procedure and how it would benefit them?
Patients considering a shoulder replacement should know that it’s an outpatient procedure and the recovery is quicker than many think. Patients often don’t need post-operative physical therapy. For a Reverse Total Shoulder Replacement, patients can expect to wear a sling for one week, and patients undergoing Anatomic Total Shoulder Replacement can expect to wear a sling for about 6 weeks.
If you’re suffering from shoulder pain and reduced joint function, schedule a consultation with Dr. Noerdlinger to find out if you’re a candidate for Exactech GPS-assisted shoulder replacement surgery. Don’t postpone getting help, so you can get back to enjoying the activities you love.