There’s nothing like being out on the water—gliding across a glassy lake on a paddleboard, navigating a winding river in a kayak, or exploring the coastline by canoe. These summer pastimes aren’t just relaxing—they’re also great for your overall fitness, building upper body strength, balance, and cardiovascular health. But like any sport, water sports come with some orthopedic risks.
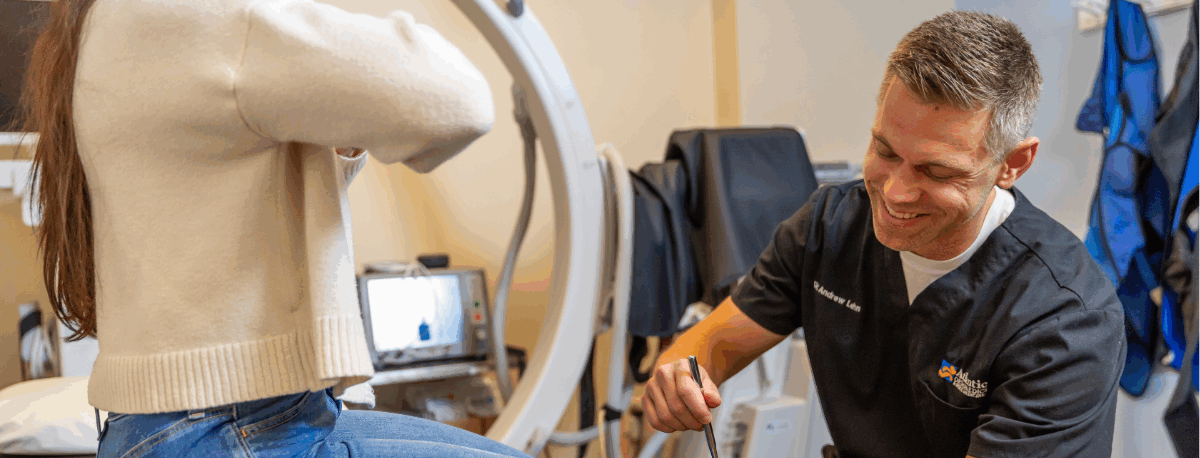
At Atlantic Orthopaedics & Sports Medicine, we see a range of water sports–related injuries every year, from overuse strains to acute trauma. The good news is that many are preventable with the right conditioning and technique—and very treatable if they do occur. Both Dr. Abigail Boduch and Dr. Andrew McMahon specialize in treating sports-related injuries and conditions, with a focus on reducing pain and getting patients back to the activities they love. Dr. McMahon has served the seacoast community as a Primary Care Sports Medicine provider and served as team physician for a number of local high school teams, while Dr. Boduch is an orthopedic surgeon (and paddle board enthusiast) who specializes in the treatment of tendon, ligament, and cartilage injuries, as well as trauma care focused on fractures of the extremities. Dr. Tyler Welch is an orthopedic surgeon and partner at Atlantic Orthopaedics who also specializes in Sports Medicine, with a focus on Arthroscopy of the knee, shoulder, and hip
Whether you’re an experienced athlete or just getting started with water sports, here’s what to watch for, how to avoid common injuries, and how we can help if something goes wrong.
Common Water Sports Injuries (and How to Prevent Them)
1. Rotator Cuff Strains and Tears
Shoulder pain is one of the most common complaints among kayakers and paddleboarders. Repeated overhead paddling motions, especially without proper technique or warm-up, can strain or even tear the rotator cuff—the group of muscles and tendons that stabilize your shoulder joint. Atlantic Orthopaedics partner Dr. Mayo Noerdlinger specializes in injuries of the shoulder, encouraging his patients to take an active role in their treatment. An advocate of opioid-sparing surgery, Dr. Noerdlinger uses novel pain-relieving treatment options to hasten the recovery process.
Prevention:
- Warm up shoulders and arms before heading out
- Use proper paddling technique—avoid overreaching or poor posture
- Strengthen shoulder and upper back muscles with resistance exercises during the off-season
Treatment Options:
- Rest, Ice, Compression, and Elevation (RICE) for minor strains
- Physical Therapy to rebuild strength and improve flexibility
- Corticosteroid Injections to reduce inflammation
- Surgical repair in the case of full-thickness tears
2. Elbow Overuse Injuries (Including Tennis Elbow)
Holding a paddle for extended periods, especially with a tight grip or poor wrist alignment, can cause overuse injuries like tennis elbow (lateral epicondylitis), which involves inflammation of the tendons around the elbow. Hand and upper extremity surgeon Dr. Maximilian Meyer has years of expertise in treating both acute elbow injuries and chronic conditions. His philosophy centers on listening to and working together with patients to create individualized care plans – both surgical and non-surgical – that help you return to an active lifestyle as quickly as possible.
Prevention:
- Avoid a death grip on the paddle—relax your hands
- Strengthen forearm muscles with light weights or resistance bands
- Mix up your activities to avoid repetitive strain
Treatment Options:
- Rest and anti-inflammatories
- Elbow braces or straps to relieve strain
- Physical Therapy with eccentric strengthening exercises
- Steroid or PRP injections for more stubborn cases
- Elbow surgery in the event of serious injury
3. Foot and Ankle Injuries
From the sudden jolt of a fall from a jet ski to the subtle wear-and-tear of beach running, your feet and ankles take a beating during many popular water sports. These joints are crucial for balance, propulsion, and impact absorption—making them particularly vulnerable in fast-paced or high-impact environments like surfing, jet skiing, waterskiing, and beach volleyball. From ankle sprains to Achilles tendon tears to “Turf Toe” (a sprain of the big toe joint), ankle and foot injuries are some of the most common when it comes to water sports.
Prevention:
- Warm up and stretch before getting on the water
- Wear appropriate footwear (water shoes, board shoes, or sport-specific bindings)
- Strengthen foot and ankle muscles with balance exercises, heel raises, and resistance band work
- Be cautious on wet, slippery surfaces—many injuries happen on docks, boats, or shorelines
Treatment Options:
- RICE (Rest, Ice, Compression, Elevation)
- Ankle bracing or taping for support during recovery
- Immobilization in a boot or cast
- Physical therapy to restore strength and stability
- Surgical repair in cases of severe ligament tears
4. Lower Back Pain and Muscle Strain
Poor posture, weak core muscles, or long hours kneeling or sitting can lead to lower back discomfort—especially for paddleboarders and kayakers. Water sports like wakeboarding and waterskiing can also result in muscle strain or injury. If you suffer from persistent lower back pain, there are non-surgical treatments that can help. Dr. Andrew Lehn is a board-certified interventional pain management provider uses spinal injections and other interventional and opioid-sparing treatments to alleviate back pain and get patients back to doing the activities they love.
Prevention:
- Incorporate core exercises like planks, bridges, or Pilates into your regular routine
- Sit tall while paddling and avoid slouching
- Alternate between sitting, kneeling, or standing to give your back a break
Treatment Options:
- Heat or ice, depending on the cause of pain
- Physical Therapy focused on core strength and flexibility
- Spinal Injections to alleviate pain
5. Wrist and Hand Injuries
Whether you’re gripping the throttle of a jet ski, maneuvering a sailboat, or paddling your way through a river, your hands and wrists are working hard. These small but essential joints are involved in nearly every water sport—and because of that, they’re also vulnerable to overuse, strain, and acute injury. If hand or wrist pain is persistent, worsening, or accompanied by numbness, weakness, or swelling, it’s important to get a proper diagnosis. Dr. H. Matthew Quitkin specializes in treating conditions of the hand and wrist, including fractures, tendon injuries, nerve compression syndromes (Carpal Tunnel and Cubital Tunnel), and overuse syndromes (Tendinitis, Tennis Elbow).
Prevention:
- Adjust your grip—keep wrists neutral and avoid bending too far forward or back
- Take breaks to shake out and stretch your hands
- Use ergonomic paddles, grip pads, or sailing gloves
Treatment Options:
- Wrist splints to reduce movement
- Ice and anti-inflammatory medication
- Corticosteroid injections for inflammation
- Surgery for persistent carpal tunnel syndrome
6. Knee Pain and Meniscus Injuries
Jet skiing, surfing, and waterskiing can all place stress on your knees. The knees act as shock absorbers and stabilizers, constantly adjusting to shifts in motion and impact from waves, jumps, and turns. A rapid pivot, a forceful landing, or an unnatural twisting motion—such as falling while your foot is still anchored in a waterski or planted during a hard turn—can tear the meniscus. In some cases, these movements may also strain or injure surrounding ligaments, like the ACL (anterior cruciate ligament), or cause patellofemoral pain syndrome, which involves irritation under the kneecap. If pain or swelling in the knee persists, don’t ignore it. Early treatment can make a significant difference in recovery. Dr. Michael Morwood is an expert in treating knee conditions, including fractures and injuries due to trauma. And Dr. Akhil Sastry is an orthopedic surgeon specializing in partial and total knee replacement. Dr. Sastry was among the first 15 surgeons worldwide to perform a robotic-assisted total knee replacement and has since performed the surgery over 1,000 times.
Prevention:
- Strengthen the muscles that support your knees—quads, hamstrings, and glutes
- Practice proper landing mechanics, and use well-fitting equipment, including bindings or knee supports if needed.
- Stretch hips and hamstrings to improve mobility and reduce strain
Treatment Options:
- Rest and elevation for swelling
- Targeted rehab exercises with a physical therapist
- MRI evaluation for suspected structural injury
- Arthroscopic surgery for severe meniscus tears
When to See a Specialist
Many water sports injuries start small—but they can become serious if they aren’t evaluated. If you experience persistent pain, numbness, swelling, or weakness after water sports, it’s time to check in with an orthopedic provider. Early diagnosis and treatment can keep minor issues from turning into long-term problems.
At Atlantic Orthopaedics & Sports Medicine, our entire team of doctors, physician assistants, and support staff are here to help get your body back in motion and feeling great so you can enjoy a pain-free summer season. From conservative treatments like physical therapy and injections to advanced surgical options, we’ll create a treatment plan tailored to your activity and goals.
Love the water? We’ll help you stay strong, safe, and ready for your next adventure. Schedule an appointment today.