Click HERE to read the entire Portsmouth Regional Hospital Article.

For more than 30 years, our very own Dr. Glen Crawford and his wife Dr. Sue Abkowitz have been spending a few weeks to a few months each year volunteering their time in countries such as Indonesia, Bhutan, Vietnam, South Africa, Ethiopia, Kenya and Tanzania.
They have built clinics, sent many 40-foot containers of medical equipment, supported educational and environment programs, developed sports programs and much, much more.
They recently were highlighted and interviewed for Portsmouth Regional Hospital’s Employee Spotlight to share about their adventures.
We are so grateful to have a humanitarian like Dr. Crawford on our team!

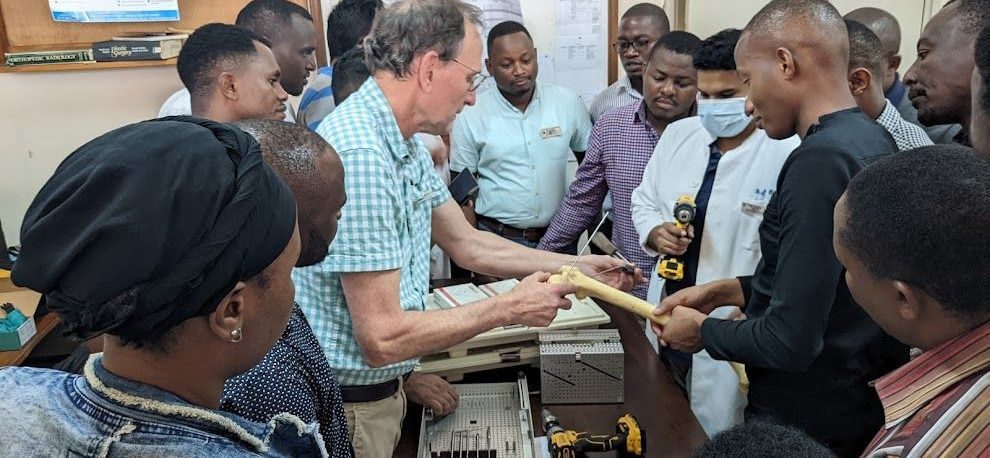
Dr. Glen Crawford is a board-certified orthopedic surgeon specializing in trauma and fracture care. Since joining the practice in 2011, he has continued to offer exceptional service to Seacoast residents. In 2003, Orthopaedics Overseas (a division of HVO, Health Volunteers Overseas) awarded Dr. Crawford the prestigious “Volunteer Surgeon of the Year Award” in recognition of his extensive volunteer work in Tanzania. He has since traveled there over 17 times, providing patient care and introducing orthopedic technology to local physicians and hospitals.
As a result of his hard work and dedication to patient care, Dr. Crawford was named a Top Orthopedic Surgeon by New Hampshire Magazine in 2022.