When it comes to orthopedic care, residents of Dover and the surrounding areas have plenty of options to choose from. But if you’re looking for a practice that delivers a unique combination of multispecialty expertise, compassion and patient-focused care, Atlantic Orthopaedics & Sports Medicine stands out. With a team of surgeons and specialists who treat the full range of orthopedic issues, including fractures and trauma, arthritis, pain management, and arthroscopic and joint replacement surgeries, AOSM offers an unmatched level of comprehensive care.
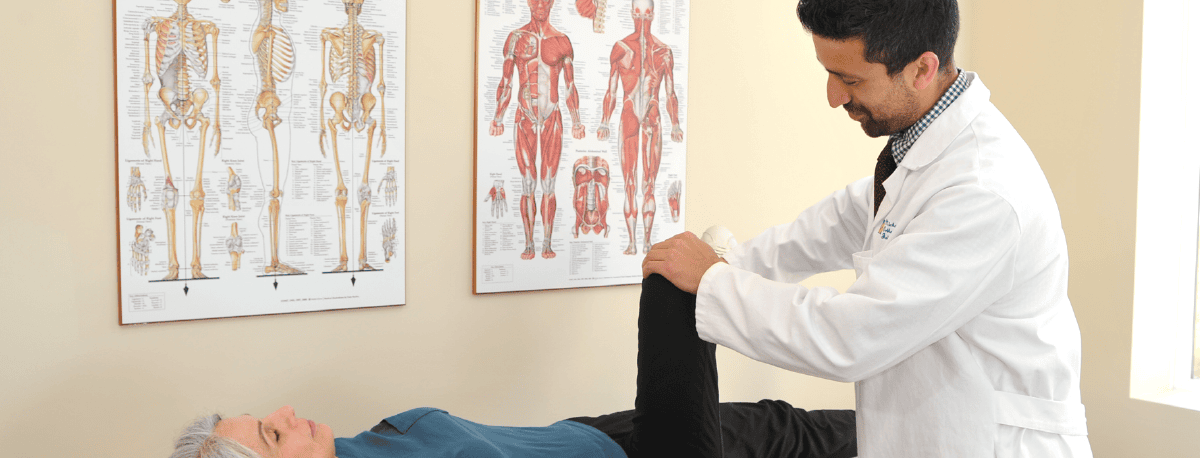
Unlike other practices that may focus on one or two areas like knees and hips, our highly skilled team brings a diverse range of specialties that cover the entire musculoskeletal system–from the neck and spine to shoulders, elbows and wrists, to knees, hips, feet and ankles. Our orthopedic surgeons bring a wealth of knowledge gleaned from top universities, world class residencies, and prestigious fellowships. Knee and hip specialist Dr. Akhilesh Sastry is recognized as the first surgeon to perform a robotic-assisted total knee replacement in New Hampshire and was among the first 15 surgeons to perform the operation worldwide. The newest addition to our team, Dr. Abigail Boduch, completed her Orthopedic Surgery Residency and Orthopedic Trauma Fellowship at Brown University, a Sports Medicine Fellowship at the University of Pittsburgh, then served as assistant team physician to the Pittsburgh Steelers before returning to her home state of NH to join our practice. This breadth of experience means that patients receive complete, cohesive care in one place, ensuring that treatment is coordinated between providers and handled by someone who truly understands their unique condition and goals.
Another benefit that sets Atlantic Orthopaedics apart is the level of care and compassion our team offers. As the largest physician-owned orthopedic practice in New Hampshire, we are uniquely equipped to prioritize patient experience. When physicians, rather than executives, determine how a practice is run, it fundamentally changes the approach to care, allowing for a more personal touch. Our doctors themselves shape the way care is delivered and have put systems and processes in place that put patients first. From consultation to treatment to recovery, our team is dedicated to providing the best possible patient experience, while maintaining the highest standards of medical care.
Choosing Atlantic Orthopaedics means choosing a practice that’s genuinely invested in the well-being of every patient. It means being treated by the best doctors around, whose comprehensive expertise and commitment to compassionate care truly sets them apart. We believe in taking the time to really listen to our patients, to understand their unique needs, so we create a treatment plan that aligns with their goals and lifestyle. Whether you’re an athlete dealing with a sports injury or someone managing chronic joint pain, Atlantic Orthopaedics is here to provide the care and support you need to feel your best. Contact us to learn more about how we can help you get back to doing what you love, pain-free.
To stay updated on announcements and our opening date at the new Dover location, sign up for our email list here!
Read what our patients have to say:
“Recently had my 2nd hip replacement procedure by Dr. Sastry and Dr. Cusson. These guys do a great job! Was again impressed by their expertise. Also, all staff associates at their surgical center were terrific. Like my 1st operation, I’m hoping to be back on the tennis court within 10 weeks. Thank you Atlantic!” – Steven G.
“You will not find a doctor better than Dr. Lehn. Always makes you feel comfortable about the procedure you are having and always takes the time to answer your questions. So grateful to have his expertise in treating my back issues.” – Joanne P.
“Doctor McMahon is great. He spent time explaining the procedure, listened and answered all my questions. It was an excellent experience.” – Ed P.